Do Statins Inhibit Cognition in Patients with Alzheimer's?
The Alzheimer’s Hub of Hope has four sections: Heroes, Highlights, Headlines and Helpers/Caregivers. This post is aligned to the headlines section.

I spend a fair amount of time canvassing the internet for Alzheimers articles, stories and research and came across research in Pubmed that determined the impact of statins on the cognition of Alzheimers patients. Statins are widely prescribed and are used to lower cholesterol.
The research“found an improvement in cognition with discontinuation of statins and worsening with rechallenge. Statins may adversely affect cognition in patients with dementia.”
The subjects of the study were Alzheimers patients taking a statin. The trial was very simple. Each subject would have their cognition assessed using the Mini-Mental State Examination three times: at the beginning, after six weeks of being off of the statin, and six weeks after the statin was reintroduced (rechallenged).
Cognition improved when not taking the statins for six weeks and worsened when assessed six weeks after the drug was reintroduced. The study can be found here.
This FDA site publishes Adverse Event Information for statins which I copied below.
Information about the potential for generally non-serious and reversible cognitive side effects (memory loss, confusion, etc.) and reports of increased blood sugar and glycosylated hemoglobin (HbA1c) levels has been added to the statin labels. FDA continues to believe that the cardiovascular benefits of statins outweigh these small increased risks.
This supports the case that statins may negatively impact cognition but states that the cardiovascular benefits outweigh this risk. It is implied that if a person is prescribed a statin they must have high enough cardiovascular risk to offset the cognitive risk.
Another study concluded cholesterol medications double your dementia risk. They took two groups of people with mild cognitive impairment (MCI) and followed them for eight years. One group was taking statins during the study while the other was not. The statin taking group were twice as likely to have their MCI develop into Alzheimers.
A YouTube video explaining this study can be found here and includes the specific name brands of medication to avoid. You may want to check this out if you are taking a statin or have concern for somebody else.
To be fair, I did come across articles and opinions that dispute the above conclusions.
When is a Care Receiver Likely to be Prescribed a Statin?
Although everybody is unique and doctors will consider many factors before prescribing a statin, it is likely to be prescribed if total cholesterol is 200 or above or LDL cholesterol is above 100.
The Cleveland Clinic’s view on this is:
Your cholesterol numbers show how much cholesterol is circulating in your blood. Your HDL (“good” cholesterol) is the one number you want to be high (ideally above 60). Your LDL (“bad” cholesterol) should be below 100. Your total should be below 200. Talk with your provider about what your results mean for you and how to manage your cholesterol.
I’m Confused, is Total Cholesterol of 240+ Ideal?
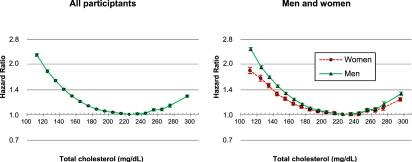
As I was going through Pubmed, I came across research that analyzed total cholesterol and its impact on mortality. The study was performed in South Korea using health records of 12+ million people from 2001 - 2004 and followed them through 2013. During that period over 690,000 people in the study died. The beauty of this study is that it is based on actual medical records and doesn’t rely on survey or anecdotal data.
The graphs below show the lowest mortality rate is at the 240 total cholesterol level. Mortality increased below and above this level.
It is interesting that the Cleveland Clinic refers to a total cholesterol of 240 and above as “dangerous” which contradicts this study which associates 240 with the lowest risk of death. Also, a total cholesterol of 300 which is considered very high has the same mortality rate as about 160 which is considered heart healthy.
I don’t claim to know why this is but it could be because the Clinic’s data is specific to cardiac risk and the Korean study is for all cause mortality which includes cardiac risk and more.
It also could be that cholesterol is part of the immune system and if it is artificially suppressed the immune system is suppressed with it which could allow for other diseases to develop. But I really don’t know and don’t have a license to be right.
The study categorizes its results by age group which you may find interesting. The study can be found here.
My Thoughts
At the risk of going against conventional wisdom, it seems to me that since a total cholesterol of 240 has the lowest all cause mortality rate, I wouldn’t take a statin to lower it to under 200 which would have the possible side effect of negatively impacting my cognition and increasing my likelihood of death. In fact, my total cholesterol is 203 and my doctor suggested I go on a statin which I refused and he didn’t push back.
My opinion is that statin users with Alzheimers or other cognitive impairment should work with their doctor to consider temporarily discontinuing the medicine in order to monitor changes in cognition. If improvements are meaningful, a risk assessment should be performed to determine whether permenant discontinuance is the best approach moving forward.