Frontotemporal Dementia (FTD) Maybe Misdiagnosed as Alzheimer's
The Alzheimer’s Hub of Hope has four sections: Heroes, Highlights, Headlines and Helpers/Caregivers. This post is aligned to the headlines section.
I received a request from subscriber Shelby to post on Frontotemporal dementia. I did some investigating and found out that this is the disease that celebrities Bruce Willis and Wendy Williams are suffering from. Willis was diagnosed at age 67 and Williams at age 59.
Many people, even medical practitioners, confuse FTD with AD since it is a type of dementia that typically occurs later in life (although often earlier than AD) and is relatively rare with only 50,000 sufferers in the United States compared to 6.7 million for AD per ChatGPT.
Because of frequent misdiagnosis, Deborah Kan, one of my Alzheimer’s Heroes of Hope, has updated her Being Patient site to include a ~10 minute FTD interactive learning guide which can be found here and a deep dive page that can be found here.
The Association for Frontotemporal Degeneration (AFTD) is linked here and has a wealth of information. On its home page it highlights the differences between FTD and AD and discusses how FTD is often misdiagnosed as AD; taking 3.6 years on average to get an accurate diagnosis.
I find it interesting that AFTD has downloadable 2-page FTD diagnostic PDFs (1 PDF per variant) where the first page is completed by the sufferer (or their caregiver) and the second page gives instructions to the healthcare provider on how to interpret the first page. Apparently, the AFTD people believe that doctors need guidance in making a correct diagnosis. The checklists are linked here and here.
Below I’ve summarized what I think are the most relevant and interesting FTD facts from Being Patient, AFTD and other resources (many of them linked below). For those who want a deep dive you are encouraged to view the sites and links yourself.
FTD Summary
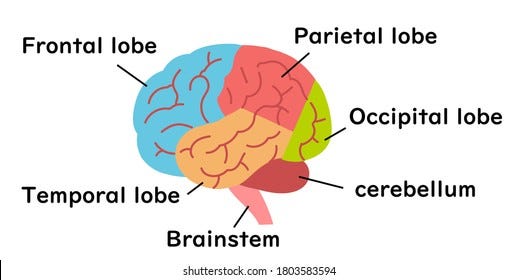
FTD is brain atrophy / shrinkage of the frontal and temporal brain lobes. Nobody knows why this occurs.
Amyloid and tau proteins are linked to alzheimer’s disease but only tau is associated with FTD.
PET (brain scans) do not show the same reduction in brain metabolism as in AD.
In many cases genetics play a role in developing FTD but it’s not the same APOE 4 variant that is associated with AD. FTD genetic testing is only available through a medical professional (not 23andme).
The onset of FTD is earlier than AD; typically from 45 to 64 years of age.
FTD impacts behavior, emotions and speech. Unlike AD, memory issues are not significant.
FTD is often misdiagnosed as AD or depression or other illnesses.
A FTD sufferer typically lives 7 to 13 years with the disease. The most common cause of death is pneumonia.
There is no cure or treatments to slow or stop the progression.
FTD Overview
FTD is a group of brain disorders caused by degeneration of the frontal and/or temporal lobes of the brain. Per ChatGPT the frontal lobe’s primary function is motor control, executive function (decision making, reasoning, impulse control), speech production and emotional regulation. The temporal lobe’s functions include: hearing & auditory processing, language comprehension, and the recognition of faces and objects. By contrast, AD typically starts in the hippocampus and progress to other areas of the brain over time.
There are two variations of FTD, Behavioral (bvFTD) and Primary Progressive Aphasia (PPA). Aphasia is a medical condition that impairs a person's ability to use or understand words.
Behavioral (bvFTD)
Behavioral variant FTD (bvFTD) is the most common form of FTD.
The hallmarks of BvFTD are personality changes, apathy, and a progressive decline in socially appropriate behavior, judgment, self-control, and empathy. Unlike in Alzheimer’s disease, memory is usually relatively spared in bvFTD. People with bvFTD typically do not recognize the changes in their own behavior, or exhibit awareness or concern for the effect their behavior has on the people around them.
As I read the typical FTD signs and symptoms below, I realized that I thought many of these were common Alzheimer’s behaviors. I’m sure I’m not the only one.
Typical signs or symptoms of bvFTD are:
Disinhibition: A loss or lack of restraint based on social norms, leading to inappropriate behavior and impulsivity. Behaviors may include:
Making uncharacteristic rude or offensive comments
Ignoring other people’s personal space
Shoplifting, reckless spending
Touching strangers or inappropriate sexual behavior
Aggressive outbursts
Apathy: Indifference or lack of interest in previously meaningful activities. Behaviors may include:
Loss of interest in work, hobbies, and personal relationships
Neglect of personal hygiene
Loss of initiative
Emotional Blunting: Loss of warmth, empathy, or concern for others. Behaviors may include:
Indifference to important events (e.g., death of a family member or friend)
Failure to recognize that loved ones are upset or unhappy
Compulsive or Ritualistic Behaviors: Single behaviors or routines that are performed over and over. These may include:
Repeating words or phrases
Hand rubbing, clapping
Re-reading the same book over and over again
Hoarding
Walking to the same place at the same time every day
Changes in Eating Habits or Diet: Excessive, compulsive or inappropriate eating & drinking, or other pronounced changes in dietary preferences.
Binge eating
Carbohydrate craving
Eating only specific foods
Increased or first-time use of tobacco products
Hyperorality (biting, chewing, mouthing)
Excessive water or alcohol consumption
Attempting to consume inedible objects
Deficits in Executive Function: Poor decision-making, judgment, problem-solving, and organizational skills. Examples include:
Difficulty planning the day’s activities
Questionable financial decisions
On-the-job mistakes that may be uncharacteristic
Primary Progressive Aphasia (PPA)
Primary Progressive Aphasia (PPA) is characterized predominantly by the gradual loss of the ability to speak, read, write, and understand what others are saying. The Merriam-webster dictionary definition of aphasia is the impairment in the use of words.
PPA is diagnosed when three criteria are met:
There is a gradual impairment of language (not just speech).
The language problem is initially the only impairment.
The underlying cause is a neurodegenerative disease.
Experts further subdivide PPA into three clinical subtypes based on the specific language skills that are most affected.
Nonfluent/Agrammatic variant (nfvPPA): Sufferers find it increasingly difficult to speak yet can still recall the meanings of individual words.
Semantic variant (svPPA): People with semantic variant PPA progressively lose the meanings of words.
Logopenic variant (lvPPA): People with logopenic variant PPA have difficulty finding words when they are speaking.
Often the sufferer will progress from one subtype to having all three.
Genetics Overview
There appears to be a genetic component with FTD, however, it isn’t APOE 4 which is often linked to AD. Therefore, the services like 23andme which evaluates APOE 4 status is not relevant for a FTD evaluation.
FTD genetic evaluations can be obtained by your doctor through companies like GeneDX. Here’s a link to their FTD genetic testing offerings.
Familial FTD
Approximately 40% of people diagnosed with FTD have a family history of one or more blood relatives diagnosed with FTD or a related condition (such as ALS), a mental health condition like depression or anxiety, progressive challenges with language or movement, or another dementia. This is referred to as familial FTD.
Genetic FTD
In a portion of those with familial FTD, a genetic variant (or mutation) can be identified as the cause: an affected parent has passed a genetic variant associated with FTD to their child. All known genetic forms of FTD are inherited in an autosomal dominant manner, meaning the child of a person with FTD has a 50% chance of inheriting the FTD-causing variant. Variants in more than a dozen genes can cause FTD; however, the most common genes are C9orf72, GRN, and MAPT. Researchers continue to discover new genes that can cause FTD.
Sporadic FTD
In approximately 60% of people diagnosed with FTD, there is no one else in the family with FTD or related conditions. We refer to this as “apparently sporadic FTD.” In these individuals, the cause of their FTD is not yet understood. A genetic evaluation should still be considered because a small number of people with no family history have a genetic cause.
Diagnosing FTD
FTD is frequently misdiagnosed as Alzheimer’s, depression, Parkinson’s disease, or a psychiatric condition.
With the exception of occasional genetic causes, today there is no single test that can diagnose FTD with certainty. The diagnosis of FTD requires a thorough history, verified by a caregiver, and a neurological examination.
As with other degenerative diseases, FTD presents an insidious onset and progresses over time. When the diagnosis is uncertain, referral to a neurologist with an interest in cognition and behavior and/or a geriatric neuropsychologist is indicated.
All patients should be screened for obstructive sleep apnea (OSA), as executive dysfunction and behavior changes are common in OSA.
Blood work should be done to exclude alternative causes of cognitive symptoms, including a basic metabolic panel, CBC, RPR, ESR, B12 level and thyroid studies.
As I do my research on AD and dementia, it is interesting to me how often B12 and thyroid deficiencies are linked to the diseases. I’ve previously posted how correcting these deficiencies can dramatically improve the condition. Note, natural B12 only is present in animal based foods. You may want to look at the embedded video in this post for a example of how B12 deficiency can look like dementia in a person.
When a family history is positive, genetic testing of the diagnosed patient can be undertaken. It is recommended that the individual see a genetic counselor first, to be sure they understand the implications of this testing.
Brain imaging can be used to rule out non-FTD conditions and may help support an FTD diagnosis. Amyloid identification during a brain scan is used to rule out an FTD diagnosis since amyloid buildup is AD indicator and not a FTD indicator.
Treating FTD
As of now, no disease-modifying treatments have yet been approved by the U.S. Food and Drug Administration.
There is no available medication or treatment that has been proven to prevent, cure or slow the decline of these disorders.
However, many FTD symptoms can be treated. Both pharmacologic and behavioral interventions are available for symptomatic benefit of specific cognitive and behavioral features including Selective Serotonin Reuptake Inhibitors (SSRI), Antipsychotic Agents and Cholinesterase Inhibitors.
Since the medication management of this patient group is complicated, primary care physicians may want to refer FTD patients with behavior problems to academic centers specializing in FTD.
Non-pharmacological interventions – including occupational therapy, physical therapy, speech therapy, and environmental changes, are the most effective interventions available today.
Managing Symptoms
Since there currently aren’t any approved treatments for the disease and managing symptoms with medicine is only so effective, AFTD has crafted self-help written and video guides addressing symptom management. Each bullet-point topic below has one or more guides that provide recommendations on the best way(s) to handle the symptom.
Click here to access the page and scroll down to the bottom for links to the symptom guide of interest.
Advanced FTD
Aggressive Behavior
Anosognosia (Lack of Insight)
Apathy/Lack of Motivation
Communication
Compulsive or Ritualistic Behaviors
Driving and FTD
Hyperoral Behaviors (preoccupation with chewing, biting, sucking, or swallowing)
Incontinence
Loss of Empathy or Emotional Blunting
Resistant Behavior
Roaming
Sexual Behavior
Sleep and FTD
Falls and Difficulty Swallowing (Dysphagia)
FTD Resources
Neuroscience: Frontotemporal Dementia (FTD) (2 min video)
What Is Frontotemporal Dementia? FTD Types, Symptoms, and Diagnosis (3 min video)
What is Frontotemporal Dementia? (5 min video)
The Difference Between Alzheimer's and Dementia: Being Patient Talks to Brad Dickerson (8 min video)
AFTD Webinar: Differentiating Behavioral Variant FTD from Alzheimer’s and Other Disorders (1 hour video)
Person-Centered Care for bvFTD: Managing Symptoms and Providing Supportive Care (1 hour video)
Maximizing Communication, Maintaining Connection — Person-Centered Care for PPA (1 hour video)